CHAMP SOFTWARE BLOG
Learn best practices for electronic health records (EHR) management in public health agencies, community health departments, and health and human services agencies, and learn how to effectively implement public health software solutions to create care pathways, track clinical data and manage resources. Subscribe to future blogs.
Featured Blog Post
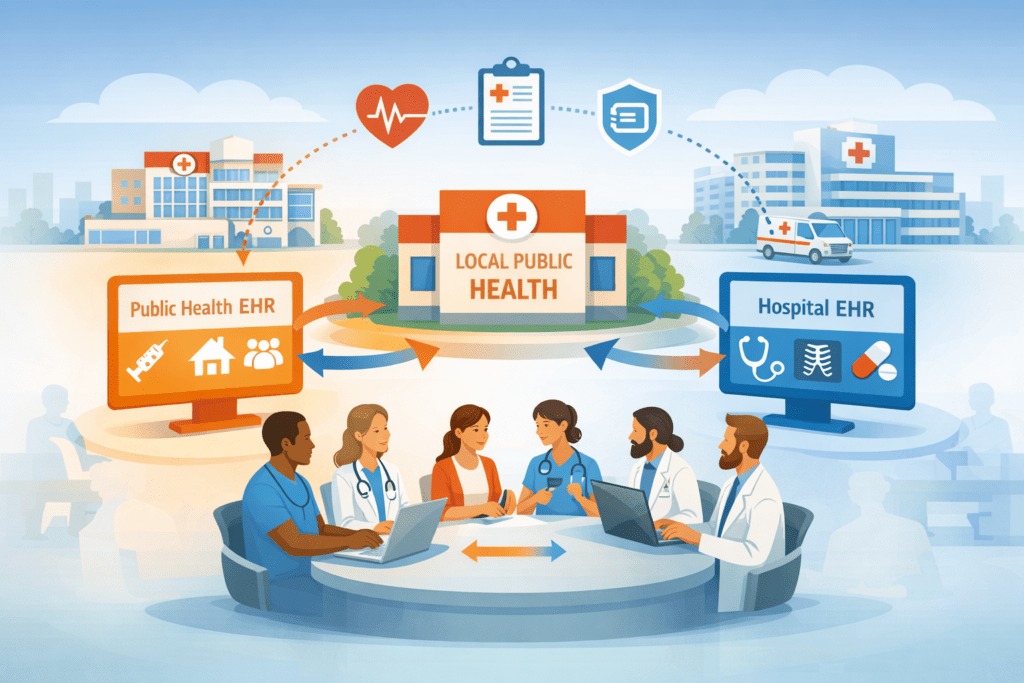
Statewide EHR Decisions are a Big Opportunity – When Local Public Health is Fully Supported
Statewide EHR Modernization Works Best When Local Public Health Has a Seat at the Table. The best approach is two systems, hospital and public health that share data.
More Blog Posts

What is a Public Health EHR
Article answers the question, What is a public health EHR? A Public Health EHR (Electronic Health Record) is a designed to support public health agencies in managing patient and population-level data. Unlike traditional EHRs that document individual clinical encounters, Public Health EHRs emphasize population health, disease surveillance, regulatory reporting, and community-wide care coordination.

Standardized Language: Importance for EHRs and Public Health Documentation
The Omaha System provides a holistic, interdisciplinary structure that covers environmental, psychosocial, physiological and health-related behavior. For EHRs, standardized languages, like the Omaha System, improve data quality, interoperability, outcomes measurement and reporting.

Adverse Childhood Experiences and Their Impact on Long-Term Health: Through a Public Health Lens, Part 2
Public health workers, especially with a strong EHR, can take actions to prevent, mitigate and measure Adverse Childhood Experiences (ACEs) which have long-term negative health impacts.
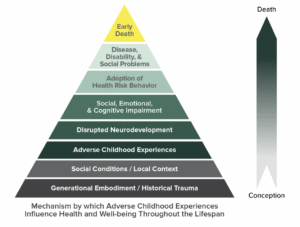
Adverse Childhood Experiences and Their Impact on Long-Term Health: Through a Public Health Lens, Part 1
Adverse Childhood Experiences impact long-term health. Documentation of ACEs screenings can help identify patterns and provide actionable insights.

Redefining Value — When an EHR Becomes a Public Health Improvement Tool
Part 4 in a 4 part series on how Webster County found Unexpected Wins with their Public Health EHR, Nightingale Notes.

Seeing the Whole Picture — Grant Management, Reporting, and Data Visibility in One System
Part 3 in a 4 part series on how Webster County found Unexpected Wins with their Public Health EHR, Nightingale Notes.

A Platform for Connection — How a Public Health EHR Strengthened Collaboration Across Departments
Part 2 in a 4 part series on how Webster County found Unexpected Wins with their Public Health EHR, Nightingale Notes.

Unexpected Wins – How the Right Public Health EHR Solves Challenges You Didn’t Plan For
Part 1 in a 4 part series on how Webster County Found Unexpected Solutions with their Public Health EHR, Nightingale Notes.

