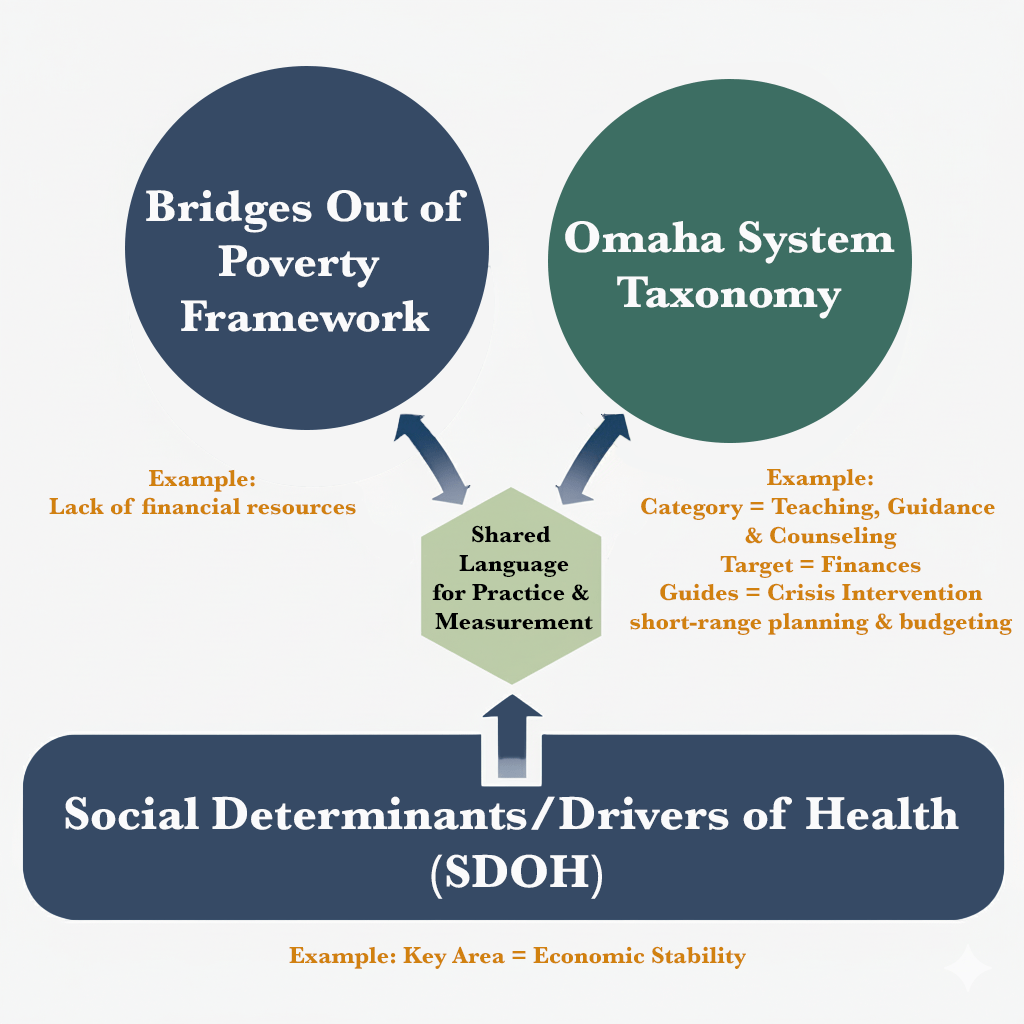
Public health teams are asked to do many things at once: meet people where they are, effect change, and prove it with data. When you combine the Bridges Out of Poverty framework with the Omaha System taxonomy—grounded in the social determinants/drivers of health (SDOH/SDOH)—you get a shared language for practice and measurement. This post outlines how the pieces fit and offers a pragmatic workflow you can take into the field tomorrow.
What each piece brings
Bridges Out of Poverty (Bridges)
Bridges is a set of tools and mental models that help communities understand and address the dynamics of poverty across individuals, institutions, and systems. Aha! Process describes Bridges as a “family of concepts, workshops, and products” that supports cross-sector poverty reduction efforts. (Aha! Process) Their program materials emphasize work “across multiple sectors to address root causes of poverty at the individual, institutional, community, and policy levels.” (Aha! Process).
The Bridges framework stems from Dr. Ruby Payne’s first book, A Framework for Understanding Poverty (1996). A second book by Dr. Payne expounded on the first, and from there more papers and works were published by other authors. The framework is now the basis of training and certifications. To learn more about Dr. Payne’s work, watch this video interview that introduces Dr. Payne and why she believes in the Bridges framework.
The Omaha System
The Omaha System is a standardized, research-based taxonomy that structures assessment, intervention, and outcome measurement. According to the website, it’s a “research-based, comprehensive practice and documentation standardized taxonomy designed to describe client care,” organized into an Assessment (Problem Classification), an Intervention Scheme, and a Problem Rating Scale for Outcomes. (The Omaha System)
Social Determinants/Drivers of Health (SDOH)
CDC defines SDOH as the “non-medical factors that affect health outcomes”—the conditions in which people “are born, grow, work, live, and age,” shaped by broader forces and systems (CDC). CMS further distinguishes health-related social needs (HRSN) as the “social and economic needs that individuals experience” which influence their ability to maintain health. (Centers for Medicare & Medicaid Services)
Why they’re stronger together
Shared mental models & structured data.
Bridges equips staff and partners with common language (resources, hidden rules, mental models of class) that can be mapped to Omaha System problems, targets, and outcomes. The result is person-centered work recorded in a way that supports evaluation and reporting.
SDOH focus & intervention pathways.
SDOH domains (economic stability, education, healthcare access/quality, neighborhood/built environment, social/community context) map naturally to Omaha Problem Classification areas (e.g., Income, Residence, Communication, Social Contact) and to Bridges tools (e.g., resource assessment, Getting Ahead groups). CDC’s framing makes it clear that improving health requires action on these conditions, not just clinical care. (CDC)
Measurement without losing the story.
Omaha’s Problem Rating Scale for Outcomes (knowledge/behavior/status) captures meaningful change—exactly the kind of capability-building Bridges aims for—while preserving context through structured notes and goals.
A practical workflow for public health teams
Step 1 — Screen and listen (SDOH + Bridges)
Use brief SDOH/HRSN screens to identify needs and strengths. Pair with a Bridges-informed conversation about resources (financial, emotional, mental, language, social capital, etc.). This creates a nuanced picture beyond “met/unmet need.” (Definition references: CDC SDOH; CMS HRSN. (CDC, Centers for Medicare & Medicaid Services))
Step 2 — Code the assessment (Omaha System)
Translate findings into Omaha Problem Classification terms (e.g., Income, Residence, Communication with community resources, Nutrition, Mental health). This standardization enables population analytics and cross-program comparisons. (Overview of components: Omaha System site. (The Omaha System)
Step 3 — Plan interventions using Bridges pathways
Select interventions (coaching, Getting Ahead groups, transportation support, landlord mediation, benefits navigation) and document them with Omaha Intervention Scheme categories (Teaching, Guidance, and Counseling; Case Management; Treatments and Procedures; Surveillance). Link each to an SDOH domain so you can evaluate what type of social driver work moves outcomes in your population. (The Omaha System)
Step 4 — Track progress with Omaha outcomes
Use the Problem Rating Scale for Outcomes to measure change in Knowledge, Behavior, and Status over time. This aligns closely to Bridges’ goal of increasing individual and community resources.
Step 5 — Close the loop and learn
Aggregate by SDOH domain, intervention type, community partner, and demographics to see what’s working where—and then bring those insights back to your team for quality improvement.
Example: Housing stability pathway (sketch)
- SDOH need: Housing instability (Neighborhood/Built Environment). (CDC)
- Bridges lens: Identify resource gaps; coach on landlord communication; connect to community allies.
- Omaha System documentation:
- Problems: Residence; Income; Communication with community resources
- Interventions: Case Management (housing referral), Teaching/Guidance (tenant rights), Surveillance (check-ins)
- Outcomes: Knowledge, Behavior and Status ratings improve as the client secures a stable lease, builds budgeting skills, and connects to a support network.
Technology that supports the workflow
For agencies that want this synergy “baked in,” Nightingale Notes by Champ Software is a long-standing public health EHR with the Omaha System at its core and mapped to the SDOH inside a pathways customizable to the Bridges framework. The integration of public health pathways using the Omaha System ensures data is documented, measurable and reportable and health departments see results like St. Louis County, MN’s shared story.
Tips for getting started
- Build a cross-walk. Map your common Bridges tools and local programs to Omaha Problems and Interventions and the SDOH area of focus.
- Train together. Hold short refreshers on Bridges concepts for nurses, social workers, CHWs, and data staff so language is shared.
- Start small. Pilot with one SDOH domain (e.g., economic stability) and 2–3 Omaha-coded interventions; evaluate every 60–90 days.
- Mind the outcomes. Prioritize the interventions that reflect capability growth—not just service completion by using the K-B-S ratings to highlight improvement.
- Use your data for advocacy. Aggregate outcomes by SDOH domain to show commissioners and funders where upstream investments are paying off.
References
Inline Sources (quoted)
- Bridges toolkit: “family of concepts, workshops, and products” supporting cross-sector work. (Aha! Process)
- Bridges materials span individual→policy levels: “across multiple sectors … at the individual, institutional, community, and policy levels.” (Aha! Process)
- Omaha System definition: “research-based, comprehensive … taxonomy designed to describe client care.” (The Omaha System)
- SDOH definition keywords: “non-medical factors that affect health outcomes” and “born, grow, work, live, and age.” (CDC)
- HRSN definition keywords: “social and economic needs that individuals experience.” (Centers for Medicare & Medicaid Services)
- Nightingale Notes & Omaha System: “standardized Omaha System taxonomy integrated into charting.” (Champ Software)
Works Cited (MLA)
aha! Process. Building Bridges Out of Poverty. aha! Process, n.d., https://www.ahaprocess.com/building-bridges/.
—. Bridges Out of Poverty Brochure. aha! Process, Sept. 2022, https://www.ahaprocess.com/wp-content/uploads/2022/09/Bridges-Out-of-Poverty-Brochure-FINAL-090622.pdf.
Centers for Disease Control and Prevention. “Social Determinants of Health | Public Health Gateway.” CDC, updated 2024, https://www.cdc.gov/public-health-gateway/php/about/social-determinants-of-health.html.
Centers for Medicare & Medicaid Services. “Social Drivers of Health and Health-Related Social Needs.” CMS, 2024, https://www.cms.gov/priorities/innovation/key-concepts/social-drivers-health-and-health-related-social-needs.
Centers for Medicare & Medicaid Services. “Social Determinants of Health (SDOH). CMS 2024, https://www.cdc.gov/about/priorities/why-is-addressing-sdoh-important.html
Champ Software. “Why Nightingale Notes EHR Uses the Omaha System.” Champ Software, n.d., https://www.champsoftware.com/the-omaha-system/.
—. “Tailoring the Omaha System: The Power of Pathways in St. Louis County.” Champ Software Blog, 15 July 2025, https://www.champsoftware.com/2025/07/15/tailoring-the-omaha-system-public-health-pathways/.
The Omaha System. “The Omaha System.” omahasystem.org, 2025, https://www.omahasystem.org/.
